Menopause is a natural stage in every woman’s life, yet it is surrounded by myths. Many women fear the unknown and believe misleading information. These myths can cause confusion, stress, and even delay treatment.
Menopause does not happen the same way for every woman. The experience is shaped by health, lifestyle, and age. Understanding the facts helps women understand the myths and facts about menopause.
This article clears 10 common menopause myths. It explains the truth behind them and highlights how lifestyle and medical care make this stage easier.
Myth 1 – Menopause Happens Overnight
Many women believe menopause begins at once, but that is not true. The process starts with perimenopause, a transition that can last four to eight years.
During this time, periods become irregular. Symptoms like hot flashes, mood changes, and sleep disturbances may begin.
True menopause happens only after 12 months without a period. Thinking of menopause as an overnight switch creates fear and confusion.
In reality, it is gradual, and recognising early menopause signs helps women prepare. Regular checkups with a gynecologist in Kolkata help manage symptoms during this stage.
Myth 2 – Menopause Only Affects Older Women
Menopause is often linked only to women in their 50s, but this is misleading. While the menopause age range is 45–55, some women experience it earlier.
Early menopause signs can appear before 40 due to various factors. The include-
- Genetics
- Surgery
- Cancer treatments like chemotherapy.
This is known as premature menopause. Women in their 30s can also experience irregular cycles or hormone changes.
Believing menopause affects only older women prevents younger women from seeking timely help. Regular medical advice ensures symptoms are not mistaken for other health issues.
Myth 3 – Weight Gain is Inevitable During Menopause
Many women have a question “Does menopause cause weight gain?”. Hormonal changes during menopause may slow metabolism, but weight gain is not inevitable.
The truth is, lifestyle plays a stronger role. A balanced diet, regular exercise, and sleep management can prevent unnecessary weight gain. Poor diet and inactivity are bigger factors than hormones.
Studies show women who stay active can maintain a healthy weight even after menopause. Instead of believing menopause myths, focus on diet, strength training, and walking daily. A gynecologist can also suggest safe nutrition plans to maintain weight.
Myth 4 – You Can’t Get Pregnant After Menopause Starts
There are several menopause and pregnancy myths that women think of as true. It is true that once menopause is complete, pregnancy cannot occur. But during perimenopause, ovulation may still happen.
Pregnancy is still possible during perimenopause. Menopause is confirmed only after 12 straight months without periods.
Many women are surprised to learn they can conceive during this stage. For those not planning a pregnancy, contraception is still important. Believing you cannot get pregnant earlier can lead to unplanned pregnancies.
Women who want children may need fertility guidance before menopause is complete. The gynecologist can explain safe timelines and family planning options during this stage.
Myth 5 – Hot Flashes Are the Only Symptom
Hot flashes are common, but they are not the only menopause symptoms. Women may also face other symptoms. These include-
- Night sweats
- Irregular cycles
- Vaginal dryness
- Sleep problems
- Anxiety
- Depression
- Memory issues.
Symptoms differ for every woman, and some may have none or mild symptoms. Others may experience symptoms for years.
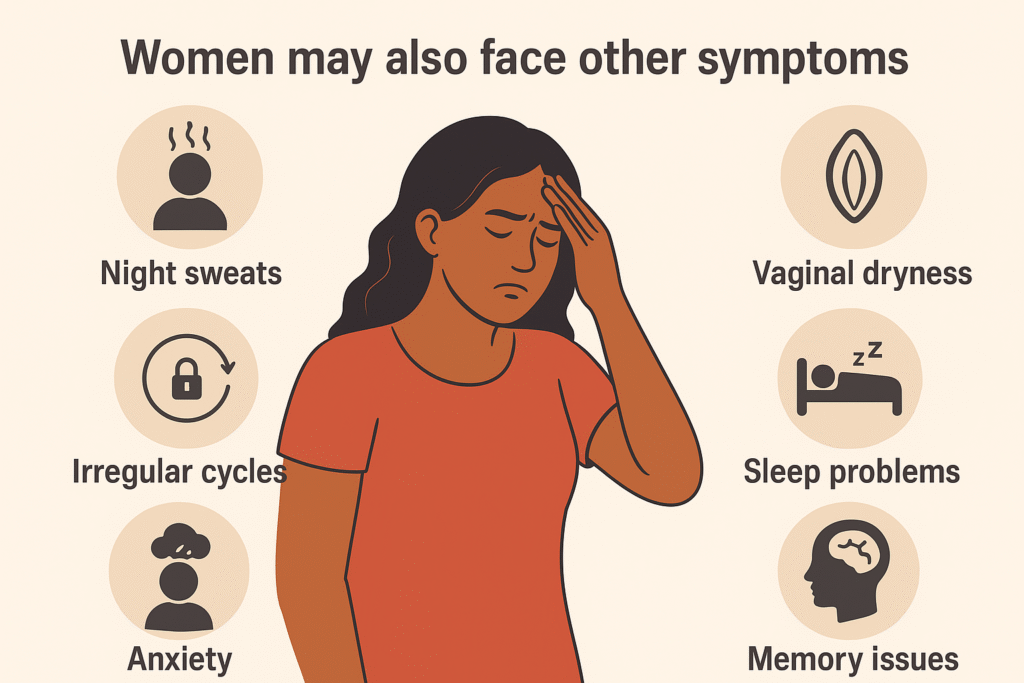
Focusing only on hot flashes makes women ignore other signs. For example, mood changes are often mistaken for stress, while they may occur due to menopause. Understanding the symptoms helps women recognise when to seek care and find relief.
Myth 6 – Menopause Always Requires Hormone Therapy
Hormone replacement therapy (HRT) is an effective treatment for severe menopause symptoms. But it is not required for everyone.
Some women manage their symptoms through lifestyle changes like exercise, yoga, or diet adjustments. Non-hormonal medicines and counselling also help.
Believing in the hormone replacement therapy myths creates unnecessary fear. This is especially because of myths about side effects.
Doctors recommend HRT only when needed and after evaluating risks and benefits. The truth is that treatment plans are personalised. The best gynecologist helps decide whether HRT, lifestyle changes, or alternative therapies are best.
Myth 7 – Menopause Means the End of Intimacy
Many women fear that intimacy ends with menopause. Vaginal dryness or discomfort is common in menopause. Medical and lifestyle solutions exist.
Simple lubricants, topical estrogen creams, and lifestyle adjustments can improve comfort. Emotional connection and open communication with a partner are even important.
If you believe intimacy ends, it can create stress in relationships. The truth is, many women continue to enjoy healthy intimacy after menopause. Menopause marks a new phase, not an end, for closeness and connection.
Myth 8 – Mental Health Isn’t Affected by Menopause
Mental health and menopause are interlinked. Hormonal shifts during menopause influence mental well-being. Women may experience mood swings, anxiety, or depression.
Stress and sleep disturbances worsen these symptoms. Ignoring this link prevents women from seeking help.
Counselling, therapy, and lifestyle adjustments help women cope better. Regular activities like walking or yoga reduce anxiety and boost mood. Support groups also provide reassurance.
Myth 9 – Natural Remedies Don’t Work
It is a myth that natural remedies never help. While not all work, some have proven benefits. A balanced diet with calcium and vitamin D protects bone health. Herbal supplements may help some women, but should only be taken with medical guidance.
Believing that natural remedies don’t work can lead women to rely solely on medicines. In truth, a mix of medical treatment and lifestyle changes is most effective. Evidence shows that lifestyle changes for menopause reduce symptoms.
Myth 10 – Menopause is the Same for Every Woman
Menopause is not a one-size-fits-all journey. Some women have mild symptoms that pass quickly, while others struggle for years.
Genetics, health, lifestyle, and age all shape the experience. Even within the same family, menopause symptoms can vary. Thinking it is the same for everyone spreads misinformation.
Understanding that experiences differ helps women prepare without fear or comparison. The best approach is the one where care is guided by the best gynecologist. Open communication helps women get the support they need. Awareness makes the journey easier.
The Role of Lifestyle in Managing Menopause
Lifestyle choices play a big role in how women cope with menopause. Exercise helps with mood, metabolism, and weight control.
A balanced diet supports bone and heart health. Avoiding smoking and alcohol lowers the risks of complications. Stress management techniques like yoga and mindfulness ease symptoms. Small, consistent lifestyle changes improve energy and sleep. This helps women feel more in control.
CASE STUDY
1. Patient Name: Mrs S
2. Age / Gender: 44 years / Female
3. Health Concern / Symptoms Reported:
Mrs S presented with irregular periods for the last 6 months. Her cycles ranged between 25–40 days. Her last menstrual period was 2 months ago. She uses condoms for contraception. She has not visited a gynecologist since her delivery. She wanted to know if this is menopause, if pregnancy is still possible, and whether irregular cycles are normal.
4. Diagnosis:
The doctor diagnosed her as being in the perimenopausal stage. This stage is the transition before menopause, when cycles can become irregular. Her TSH was normal (2 mIU/L), and FSH (8 mIU/mL) confirmed she has not yet reached menopause. Her BMI was 26, which is in the overweight range. Her blood pressure was 120/80.
5. Treatment / Advice Given:
- The doctor explained that irregular cycles are common at her age due to hormonal changes.
- Menopause has not occurred, as menopause requires 12 straight months without bleeding.
- Pregnancy is still possible, though the chances are lower. She should continue contraception if she does not wish to conceive.
- She was advised to maintain a healthy diet, regular exercise, and weight control.
- A gynecology review and pelvic ultrasound were suggested if bleeding becomes heavy or cycles stay irregular.
- Regular follow-up every 6–12 months was recommended.
6. Outcome / Result:
Mrs. S was reassured. She understood that her irregular cycles are part of perimenopause and not menopause yet. She also understood that pregnancy is still possible. She agreed to keep track of her cycles and return for follow-up if new symptoms appear.
When to See a Doctor About Menopause Symptoms
See a doctor if symptoms disturb daily life. Severe hot flashes, heavy bleeding, or depression need medical attention.
A gynecologist will rule out other health issues and suggest treatments. If early menopause signs appear, consult a doctor quickly for evaluation. Do not ignore persistent discomfort. Early help makes menopause easier to manage and improves quality of life.
Age gracefully and stronger
Menopause is not an ending. It is a transition that needs the right knowledge and care. Consult Dr. Pallab Roy, the best gynecologist in Kolkata. Trust your body, and take charge of your health.
FAQs: Age, Symptoms, and Treatments
Can menopause happen before 40?
Yes, this is called premature menopause and may be linked to genetics, surgery, or medical conditions.
How long do menopause symptoms usually last?
Symptoms like hot flashes or mood changes can last 4–8 years during perimenopause and sometimes longer.
Does every woman experience severe symptoms?
No, some women have mild or no symptoms, while others face stronger physical and emotional changes.
Can menopause affect bone health?
Yes, falling estrogen levels increase the risk of osteoporosis, so calcium and vitamin D are important.
Are there treatments apart from hormone therapy?
Yes, non-hormonal medicines, counselling, lifestyle changes, and natural remedies can reduce discomfort.